The Ultimate Ancestral Guide To Fertility
The Ultimate Ancestral Guide To Fertility
Written by Brian Johnson (Liver King)
Fertility can be traced from the inception of our species. From the beginning of creation and in all ancestral storytelling, this great concept is duly manifested. Fertility has a deep seeded relationship with the perennial human desire to survive and perpetuate his existence.
“We don’t inherit the Earth from our ancestors, we borrow it from our children.” — Native American Proverb
Nutrition giants like Weston A. Price (Nutrition and Physical Degeneration) and Sally Fallon (Nourishing Traditions & Nourishing Baby) have extensively researched and written about the importance of nourishment for fertility.
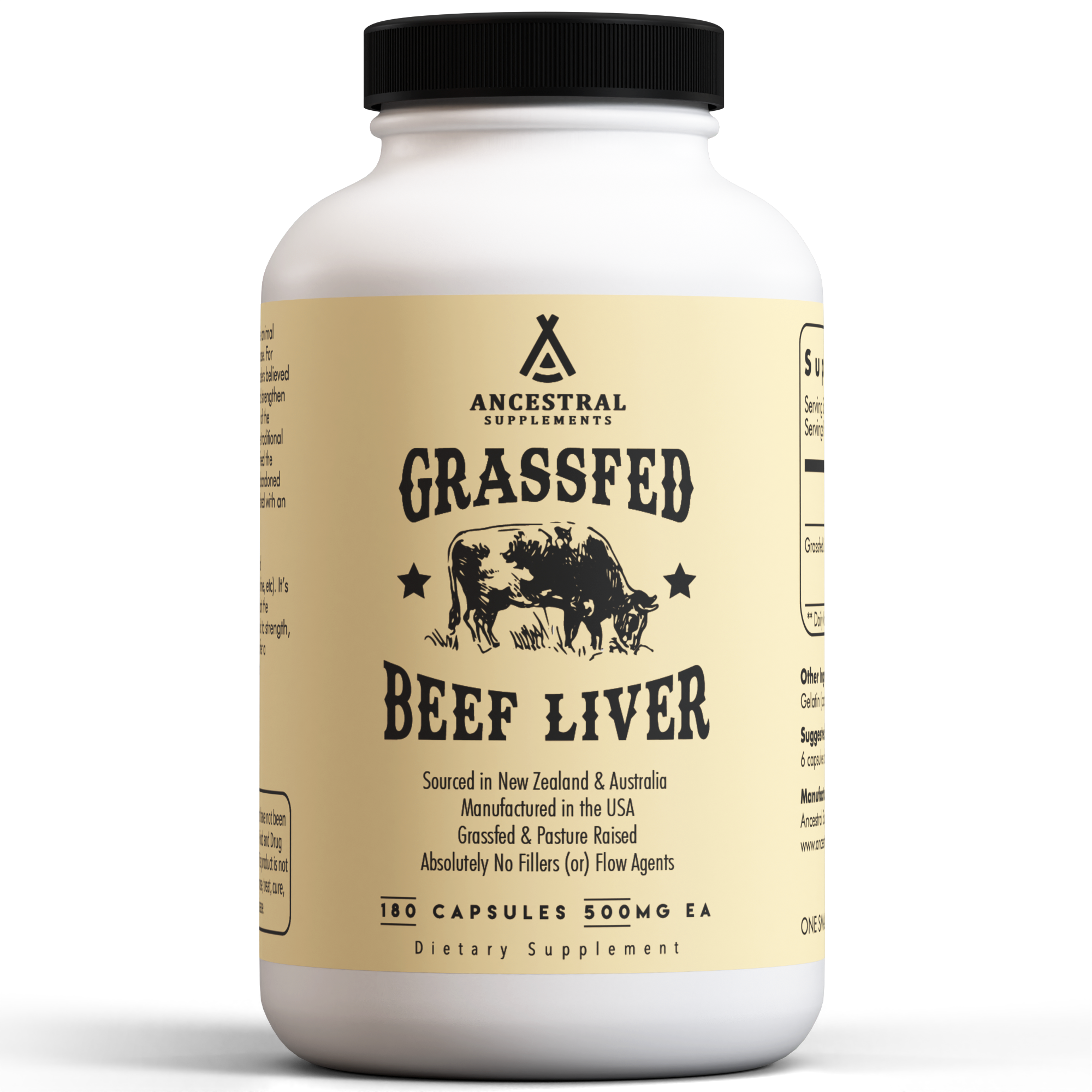
In particular, Weston A. Price discovered that certain foods, such as liver, bone marrow, fish eggs, egg yolks, and tallow, were staples in our ancestors’ diets to allow for easy conception and the creation of healthy, beautiful babies. Today, modern science tells us why. For instance, we know that healthy sperm and fertile eggs require animal-sourced vitamin A (called retinol) to function properly. Grass fed, grass finished liver is unequivocally the best source.
Many functional healthcare practitioners recommend these traditional foods in the diets of couples trying to conceive… liver and bone marrow at the very least (I know, big surprise!). And in this article, you’ll learn why — there is just something special about this combination of traditional foods. Of course, I hope that you will also consider incorporating skin-on wild fish, egg yolks, and tallow for the all-important stable omega-3 fatty acids, choline, folate and other nutrients we will discuss.
(In)Fertility in the modern world: an evolutionary mismatch
I believe that the human organism is superbly adapted to an environment that no longer exists. Our modern world is totally inappropriate for the bodies we inhabit today. Most of our health and happiness problems result from this mismatch; including the fertility narrative.
The solution is to find ways to recreate our ancestral environment in the modern world. The information presented here is meant to provide you, descendant of the sole surviving species of genus Homo (the baddest mammalian predators that ever lived) insights to reclaim your strength, health, and happiness in the modern world.
Infertility — an inability to conceive after a year of trying — is a pretty big issue, with roughly 15% of US couples considered infertile.1 It’s also not a one-sided issue, with men being responsible for a quarter of the problems.2 In fact, 3.3–4.7 million men in the USA, or about 7.5% of all sexually active men, are actively seeking help for fertility.3
There is no doubt the modern world (diet, environment and lifestyle) are to blame. The abundance of highly processed, nutrient-poor foods combined with chronic stress, poor sleep habits, and endocrine-disrupting chemicals help explain the declines in semen quality and sperm counts men have been experiencing over the last 50 years.4,5
Address estrogen dominance
Yes, I’m a man, but you’d be surprised what I’ve learned about estrogen due to how it impacted my own life. Endocrine-disrupting chemicals that favor estrogen dominance in the body are pervasive in our modern world. They have far-reaching health effects warranting concerns for both men and women. When I have this conversation with people, I always go back to the root-cause narrative.
You can’t out-supplement these chemicals. To be healthy, and to stay healthy, we need a total systems approach with diet, lifestyle, and behavior. This is because our hormones operate on mostly negative feedback loops, whereby higher levels of a given hormone down-regulate production to maintain balance. Similarly, greater exposure to hormones will down-regulate the activity of receptors they bind to, so there is less hormonal signal being seen by the body.
Hence why we need a total systems approach. Balancing estrogen naturally should be a major focus for both men and women, especially considering that almost everyone is bathing in phytoestrogens and xenoestrogens in the modern world. I know I was, ten years ago. I developed a lump in my chest, it grew, my estrogen was way higher than it should have been, I had estrogen dominance — as do many other men and women in the modern world.
I eliminated all phytoestrogens and xenoestrogens from my life, which is one reason why I talk about not eating nor drinking nor wearing from non-native materials, because this is yet another source of estrogen. I also provided my body with all the things it needs for detoxification, which includes heavily supporting liver and kidney health. Turns out, I am homozygous for the COMT gene, meaning that I have an 80% decreased capacity to clear estrogen (thanks mom and dad!). So, I further supported my methylation metabolism with lots and lots of liver and egg yolks. My estradiol (e2) went from >80 pg/mL to within 22–26 pg/mL, the lump totally went away, and my life is way, way, way better now as a result.
Once again, think root cause… and yes, this is only one of them! In biological systems, it’s rarely one (or) the other that produces results (for good or bad), but rather the combination of diet, lifestyle, and behavior.
Unhealthy diets and lifestyles
When we look at dietary patterns around the world, eating more processed meats, soy products, sugar, trans fats, coffee, and alcohol are associated with worse sperm quality.2,6,7 As is eating less vegetables and fruits, fiber, antioxidants, poultry, and omega-3 fatty acids from fish and other seafood.
Certainly, these unhealthy habits are one reason most people are overweight or obese. Thankfully, a little weight loss is associated with improvements in sperm parameters in men, and with improved chances of becoming pregnant in women.8
Stress affects about 59% of the working class, with symptoms of burnout and exhaustion being most common.9 Higher perceived stress levels are associated with reduced semen quality,10–12 meaning that it isn’t the stress that’s the issue, but how you handle it. And, hopefully, you don’t turn to alcohol or cigarettes to do that, because they are associated with reduced sperm quality too.13–15
The implications are far more pronounced than you might think, and we have Pottenger’s cats to thank for that. Francis M. Pottenger Jr. was a physician who worked with donated laboratory cats to study the transgenerational effects of diet. He fed the cats various combinations of raw and cooked meat and milk, let them breed, and repeated the experiment, documenting the effects across generations.
Because certain nutrients that cats must consume in the diet are destroyed by cooking, the cooked food cats slowly developed deformities throughout their life, like narrowed faces, frail bones, and weakened joints… does this sound familiar? They also developed numerous diseases and fertility declined. After three generations of eating a primarily cooked diet, the young kittens died before adulthood and reproduction ceased.
Notably, most everything reversed once raw foods were fed to the cats who were raised on cooked foods. Less of them died, diseases resolved, and health was restored within months. The takeaway point here being that our diet doesn’t just affect our health — it affects our unborn children’s health too.
“Pottenger’s findings should be seen in the context of Weston A. Price’s research and can be interpreted as follows: When the human diet produces “facial deformities” — the progressive narrowing of the face and crowding of the teeth — extinction will occur if that diet is followed for several generations. The implications for western civilization-obsessed as it is with refined, highly sweetened convenience foods and low-fat items — is profound.”16
Ancestral fertility
In stark contrast to the fertility issues of overabundance in today’s world, the biggest issue for our ancestors was a lack of food and lack of body fat, coupled with too much activity.17,18 The body has finite resources, and it can’t spend them on reproduction if it thinks you are starving.
The renowned scientist Bruce Ames put for the Triage Theory to explain this phenomenon.19 Essentially, short-term survival is favored over long-term health and reproduction when there is a shortage of nutrients. If you aren’t getting enough fat-soluble vitamins and minerals, as could easily happen in our ancestors’ unpredictable times, then what you do get will go towards keeping you alive, not towards fertility.
This resulted in many cultures valuing certain foods for fertility, consuming them in preparation for pregnancy. Both men and women took part — these foods were non-negotiable additions to the diet to purify the body and prepare the womb.
Weston A. Price knew early on that they were rich in mineral and fat-soluble vitamins (called fat-soluble activators at the time):
“One of the serious human deficiencies is the inability to synthesize certain of the activators which include the known vitamins… I have shown that the primitive races studied were dependent upon one of three sources for some of these fat-soluble factors, namely, seafoods, organs of animals, or dairy products. These are all of animal origin.”20
Fish eggs, shellfish, and fatty fish are rich in several fat-soluble vitamins, minerals, and essential fats. These foods were staples among the Eskimos of Alaska, the Maori in New Zealand, the islanders of Northern Australia, and the native tribes in the various archipelagos of the South Pacific.20 Even our Native American ancestors would go to great lengths to obtain fish eggs, be it through trade or their own accords:
“It was, accordingly, a matter of great interest to discover that these Indians used regularly dried fish eggs from the sea… When I inquired of them why they used this material they explained that it was necessary to maintain the fertility of their women. I was informed also that every exchange depot and market carried these dried fish eggs so that they were always available.”20
Organ meats were consumed in virtually every indigenous culture. Liver, especially, is known as nature’s multivitamin and the most nutrient-dense food on the planet. In fact, our Native American ancestors would commonly favor organ meats over muscle meat, feeding that to their dogs.
“I found the Indians putting great emphasis upon the eating of the organs of the animals, including the wall of parts of the digestive tract. Much of the muscle meat of the animals was fed to the dogs.”20
Among the organ meats, thyroid gland was especially important for fertility. Our ancestors living far North would gorge on moose thyroid glands during winter months and have most of the children born during summer months as a result. Perhaps we can learn something from them about the importance of thyroid health for reproduction.
“For the Indians of the far North reinforcement was accomplished by supplying special feedings of organs of animals. Among the Indians in the moose country near the Arctic circle, a larger percentage of the children were born in June than in any other month. This was accomplished, I was told, by both parents eating liberally of the thyroid glands of the male moose as they came down from the high mountain areas for the mating season, at which time the large protuberances carrying the thyroids under the throat were greatly enlarged.”20
Raw dairy products like fresh milk, cream, and butter were regularly eaten among cultures that herded mammals. This includes the Swiss in the high Alps, the Arabs (using camel's milk), and the Asiatic races (using milk of sheep and musk ox). The best butter comes from cows eating rapidly growing green grass in the spring and fall.
“I have referred to the importance of a high vitamin butter for providing the fat-soluble activators to make possible the utilization of the minerals in the foods. In this connection, it is of interest that butter constitutes the principal source of these essential factors for many primitive groups throughout the world.”20
Eggs and bone marrow were consumed opportunistically among those tribes that had access. After all, not all of our ancestors regularly hunted big game or scavenged for eggs. But when these foods were available, our ancestors made sure to stock up.
“It is important that skeletons are rarely found where large game animals have been slaughtered by the Indians of the North. The skeletal remains are found as piles of finely broken bone chips or splinters that have been cracked up to obtain as much as possible of the marrow and nutritive qualities of the bones.”20
Why these foods were sacred
When we look at traditional wisdom through the lens of modern nutritional science, it isn’t difficult to see why these foods were prized by our ancestors. These foods were incredibly nutritious and helped ensure that the diet contained ample calories, protein, fat, vitamins, and minerals.
Obviously, these foods contained an abundance of nutrients the body requires to thrive, but they were also incredible sources of several key nutrients the body requires for fertility, reproduction, and ensuring that the womb supplies ample nutrition to the growing baby. That’s our focus.
The Omega-3 Fatty Acids (EPA & DHA)
One of the reasons seafoods were prized by many our ancestors was because they are rich in two essential fats: eicosapentaenoic acid (EPA) and docosahexaenoic acid (DHA).21 These little guys are the reason fish oils are so popular today, since no one likes eating fish anymore (as if anything tastes better than a properly seared wild salmon fillet that’s smothered in butter, topped with fish eggs, and served with a side of guacamole).
Obviously, our ancestors didn’t always have access to fresh seafood, which is why they consumed brain and bone marrow from land animals as a staple. We spent a good chunk of time being scavengers, before evolving into the baddest mammalian predators (hunters) that ever lived. We would sit and wait… patiently… for predators to do their thing, so that we could do ours. When the coast was clear, our earliest ancestors would scurry over to the carcass, harvest the valuable bones and the skull, and crush them against rocks to gain access to the nutrient-dense brain and bone marrow.
You would be surprised how rich in omega-3s brain and bone marrow are. These ancestral sources of EPA and DHA have been lost in the modern world… seafood is not the only way to get these vital fats (nor) is it the original way that we evolved the big brains that we enjoy today.
Yes, vital — EPA and DHA are fundamental for shutting off inflammation and not letting it run wild.22–24 These effects are due to the fact that EPA and DHA serve as the precursors from which specific anti-inflammatory molecules are made.
Inflammation is known to play a role in many reproductive disorders,25 not to mention obesity, diabetes, heart disease, and other health problems that have downstream negative effects on fertility. Infertile men have lower levels of EPA and DHA in their sperm than fertile men do,26 and supplementation with EPA and DHA improves sperm quality.27
More important, though, is that eating fish, brain, and marrow sets the stage for a healthy pregnancy. DHA represents about 97% of all omega-3 fatty acids in the brain,28 and both EPA and DHA are essential for proper fetal development, including neuronal, retinal, and immune function.29,30 So, not only does obtaining ample EPA and DHA help stave off chronic inflammatory conditions and improve fertility, it also ensures you have the building blocks necessary for a healthy baby.
Retinol (the real vitamin A)
Liver is the richest source of vitamin A in the world, even today. And I’m talking about the real stuff that the body needs and uses — retinol. Yeah, plants contain compounds that the body can convert to retinol, but this process is strongly influenced by genetic factors and very unreliable.31
Vitamin A plays many important roles in the body, so it isn’t difficult to see why it is mandatory for reproduction. Most people know it plays a role in eye health (and being able to see your mate is certainly an advantage), but it is also involved in regulating the growth of virtually all cells in the body, including sperm, eggs, and the baby that ensues.32,33
Not getting enough vitamin A not only impairs the production of sperm in men and the proper development of the placenta or baby, it can prevent pregnancy altogether.34,35 Plus, it can lead to more infections and illness,36 as well of thyroid dysfunction,37 all of which can have negative downstream effects on fertility as well.38,39
Vitamin A is commonly referred to as the concertmaster because of its role in cell differentiation.
Vitamin D
Seafood, especially fish eggs, seal and whale blubber, cod liver, and fatty fish, is rich in vitamin D. Now, I know that this is the “sunshine” vitamin because we make it in our skin when exposed to sunlight. But the sun isn’t always around, particularly for people living far away from the equator. So, foods are yet another source to ensure sufficiency… so yes, eat your vitamin D!
Vitamin D is essential for bone health, but also has many non-skeletal effects, particularly on the immune, hormonal, and cardiovascular systems. The systemic role of vitamin D has some serious implications for fertility and reproduction. Vitamin D insufficiency of pregnant moms-to-be has been associated with an increased risk of gestational diabetes, pre-eclampsia, and lower birth weight infants.40
When it comes to fertility, vitamin D is essential for the development of healthy sperm, eggs, and placenta.41 Moreover, vitamin D insufficiency reduces testosterone levels and impairs ovulatory function.42–44 So, get some sun, or get some fish. Better yet, do both.
Choline and Folate
Eggs and organ meats are incredible sources of choline and folate, two nutrients that are critical for the proper development of the nervous system. Folate supplementation is already recommended during pregnancy to prevent neural tube defects of the baby,45 but choline hasn’t yet made the list despite plenty of research showing that pregnant women have an increased requirement to support the developing baby’s brain.46,47
From a fertility standpoint, ensuring both nutrients are eaten in ample quantities is important for personal health. Choline, for example, is involved in maintaining the integrity of cell membranes, allowing for cells to communicate with one another (particularly in the brain, laying the foundation for lifelong memory), and allowing for fat metabolism. In fact, one of the clear-cut signs of choline deficiency is fatty liver.48 Folate is necessary for the creation of DNA.
You also want to be sure you aren’t heading into pregnancy with an insufficiency, since many conditions such as neural tube defects occur within weeks of becoming pregnant — well before you may notice! Similarly, cognitive development of the child is incredibly reliant on ample choline availability,49 so you want those stores to be built up before conception.
Iron, zinc, and magnesium
All meats are going to be a rich source of the highly bioavailable heme iron and zinc, which are two essential minerals on opposite sides of the same coin.
For women, there is a clear link between low iron status poor pregnancy outcomes, such as low birth weight, preterm birth, and increased risk for newborn death.50 Iron requirements during pregnancy are considerably increased;51,52 yet, over 20% of women in developed countries enter pregnancy with extremely low iron stores, with figures in developing countries likely even higher.53,54
For men, zinc plays many essential functions in keeping men up-to-par, such as maintaining testosterone levels, prostate health, and sperm quality.55,56
For both, magnesium is paramount. Low magnesium status is common during pregnancy, and animal studies consistently demonstrate that this results in worse pregnancy outcomes.57 Supplementing magnesium during pregnancy has been shown in humans to reduce the frequency of preeclampsia, preterm births, low birth-weight infants, and gestational diabetes.58 Magnesium is also required for the production of testosterone in men,59 which has obvious implications for fertility.
The ultimate ancestral guide to fertility… reclaiming fertile times
Now the moment we’ve all been waiting for… the perennial human desire to survive and perpetuate our existence is hard-wired into us. Here’s the ultimate guide to doing it better:
Know your window. Ladies, you aren’t fertile 24-7. I can’t stress this one enough, knowing where you are at on your cycle can make or break a successful pregnancy. There are roughly six days each cycle where fertility is at its peak: five days before and the day after ovulation.60 This is known as the Fertile Window.
This seems obvious, right? Well, this is one of the main reasons couples are unsuccessful. Most women do not actually understand their reproductive cycles — less than 13% could accurately identify their fertile window.61,62 This is one area where modern technology can help immensely, as there are various menstrual cycle apps that can help women keep tabs on their fertile window and thereby help with becoming pregnant.63
Space your children. Okay, this one isn’t so much about fertility as it is about ensuring each baby is as healthy as they can be. Having children 18–23 months apart is suggested to have the lowest risks of adverse pregnancy outcomes, such as preterm birth, low birth weight, and low birth size.64 On the other hand, if you have suffered a miscarriage, then becoming pregnant within six months doesn’t increase the risk for adverse events and may even reduce the risk for preterm delivery or a second miscarriage.65 That said, keep in mind that Mother Nature doesn’t always follow your plans, so stay flexible and welcome each new child into your home with love.
Wait 4–6 months. Men may be making millions of new sperm every day, but they take several months to fully mature. So do eggs, which receive a signal to begin their final maturation process about 150 days before they would be released from the ovary. It is therefore paramount to wait at least four months after implementing the steps put forth in this guide to ensure that sperm and eggs are developing in a nutrient-rich environment that will optimize fertility. This is especially important if you had been using birth control, which depletes the body of important nutrients like folate and magnesium.66 Plus, remember Pottenger's cats — we don’t want to pass on bad nutrition through generations.
Ditch the chemicals. The list of chemicals we are exposed to daily is endless, from plastics to pesticides to personal care and cleaning products. These environmental toxins are all risky business when it comes to making a baby since many are hormone disruptors.67
For example, 15 of the most widely used pesticides have been shown to harm sperm quality and alter testicular function in men.68,69 Nonylphenol, a common ingredient of many cleaning products and a stabilizer in plastic food packaging, is a known reproductive toxin.70 Worse yet, these negative effects can be passed to your children.71
Also, the notion that the dose makes the poison doesn’t apply to most of these chemicals, which show harmful effects even at doses we are commonly exposed to in everyday life.72 The Environmental Working Group is non-profit resource group that can help you identify strategies to reduce your toxin exposure. Start here:
- Ovotoxins disrupt (and can out-right stop) ovulation.
- Endocrine (hormone) disruptors interfere with hormone function, including your sex hormones, which can cause endometriosis, PCOS, erectile dysfunction, and infertility.
- Phthalates are endocrine disruptors used in plastic food containers, cling wrap, IV bags, medical supplies, and vinyl flooring. They disrupt hormonal signaling at low levels, and have been associated with miscarriages and testis toxicity with greater exposures.73,74
- VCH are ovotoxin chemicals are used in rubber tires, plastics, and pesticides.75
- PAHs are chemicals released from cigarettes, car fumes, and road tar that are associated with reproductive problems in women and men.76,77 They are also produced when you cook meat at really high heats, such as pan-frying or grilling.
- Pesticides are found mostly on non-organic fruit and vegetables, with other sources of exposure being conventional meats, dairy, and unfiltered tap water.
- Formaldehyde is found in air fresheners, deodorants, floor polish, and upholstery cleaners.
- Bisphenols are found in plastic containers and can leach into food and water.
- Organic solvents are petroleum-based liquids found in household products, electronics, car repair, health care, photography, agriculture, printing, construction and cosmetics and many more.
- Dry-cleaning chemicals
- Paint fumes
Filter your water. Tap water can be full of heavy metals, pharmaceuticals, and chemical run-off that accumulate in your body and wreck havoc. Lead is an infamous one, but arsenic, copper, cadmium, atrazine, perchlorate, and PFOA/PFOS (chemical cousins of Teflon) also occur in millions of Americans’ tap water.78 And for God’s sake, stop drinking out of plastic water bottles already!
Be wary of EMFs. Radiation is all around us, and electromagnetic frequencies (EMFs) are a huge contributor. This comes from those electronics you can’t seem to live without: computers, cell phones, wi-fi, etc. Cell phones are probably the most devious considering they near necessity in today’s world. Yet, greater exposure is associated with worse sperm quality.79,80 The best things you can do are not put laptops on your lap, not keep your cell phone in your pocket, and shut off your wifi and other electronics at night when they are not in use.
NOTE: In World War II, radar operators could easily create sterility by exposing the groin to radar waves.81 Radar is microwave radiation and was the precursor to cell phones that use similar frequencies.
Limit sauna time. High temperatures have dramatic effects on the production of sperm.82 Simply using a sauna for 15 minutes twice per week reduces sperm count and motility in healthy men after three months.83 Thankfully, the effects reversed after six months of ceasing sauna treatment. Similar effects have been found with sitting in a hot tub for 30 minutes every three days over a month, which were also reversed after stopping.84 If you’re a guy interested in having kids, avoiding saunas and hot-tubs for 3–6 months before trying to conceive might be a good idea.
Get more sleep. Sleep is a cornerstone of good health, and I’ve previously written about how to reclaim healthy sleep. Check out that article on ways to optimize your sleep habits and environment. After all, poor sleep hygiene is associated with infertility.85,86
Get more sun. Sunlight exposure is important for overall health through stimulating the production of vitamin D and setting our circadian rhythms. Both play a central role in reproduction. We’ve already discussed vitamin D, which is essential for the development of healthy sperm, eggs, and placenta.41 Sunlight by way of circadian rhythms is equally important. Women are more fertile in the summer than the winter,87 and morning bright light exposure has been shown to aid fertility.88
Reduce stress. Psychological stress, anxiety, and depression can contribute to reduced odds of a successful pregnancy. It is very important to take time for yourself and slow life down if you want to have a healthy baby. Go for a walk outside (and get some sun!) or practice yoga, tai chi, or meditation — just do things you find enjoyable and relaxing.
Lose weight. If you have been growing the keg lately, now is the time to focus on a six-pack. Being overweight or obese increases the risk of being infertile and obtaining a healthy weight is associated with improvements in sperm quality in men, and with improved chances of becoming pregnant in women.8 This doesn’t mean going from one extreme to the other, since being underweight also reduces fertility, especially in women. A healthy body weight (BMI of 20–24) is optimal for a baby to grow.89
Be more active. Ensure adequate physical activity throughout the week. Our ancestors were rarely lying around, and only after being on their feet all day hunting, gathering, and taking care of their tribe. Regular physical activity not only improves overall health, but also benefits the reproductive system of both men and women.90,91 The American College of Sports Medicine recommends 150 minutes of moderate to vigorous activity per week. This is easily achieved by going for those sunshine walks, or practicing various forms of stress reduction (like yoga). It can also aid in maintaining a healthy body weight.
Say no to drugs. Smoking anything or consuming any form of tobacco are obvious, but you also need to be mindful of alcohol and caffeine. Easier said than done, right? I get it, I love my morning cup of Joe, and you don’t need to avoid it completely. Just limit yourself to 1–2 cups per day. As for alcohol, priorities. It’s a toxin, you don’t need it, and its use is associated with numerous reproductive risks.15
Eat your sacred foods. Liver and bone marrow are the fundamentals and they'll give you the most bang for your buck. A far-off second place goes to fatty wild caught skin-on, bone-in sardines, wild king salmon (also called Chinook salmon), wild fish eggs, wild cod liver, wild shellfish like oysters and mussels, and other organ meats from grass-fed cows, like brain, spleen, kidney, and thyroid. Don’t forget the bone broth, egg yolks, and raw dairy are all nutrient-dense powerhouses that will not only keep your diet in tip-top shape, but also supply key nutrients necessary for fertility and creating an optimal environment for a growing baby.
NOTE: choline causes a lifelong increase in memory and attention.
- Liver
- Bone Marrow
- Wild Fish (skin-on, bone-in) & Wild Fish Eggs
- Pastured Egg Yolks
- Raw Dairy
Minimize trans-fats. This should be a no-brainer; there is no safe level of trans-fats. We have known for a long time that trans-fats like partially hydrogenated oils are toxic. Thankfully, avoidance is rather easy, since they tend to hide in all the foods you shouldn’t be eating anyways: doughnuts, biscuits, french fries, and many other processed frakenfoods. If you do need to eat out of a box, be diligent and read the ingredients list.
Minimize conventional and pasteurized (cooked) dairy. Cow’s milk from factory farms is full of hormones and chemicals the cows soak up from their environment, which have important implications for our health.92 Do you think an excess consumption of these hormones could disrupt your own hormonal balance? You bet!
Pasteurization (cooking) destroys vital nutrients that we may not be aware of — remember Pottenger’s cats! Milk is meant to nourish a growing animal, and it provides a truckload of things to do that… healthy bacteria (probiotics), fibers (prebiotics), bioactive peptides, immune cells, etc. Cooking kills all that. There is no ancestral culture in history that cooked its milk. Now, finding raw milk isn’t always easy… I get it. If you don’t have access to a trusted farmer, check out the Weston A. Price Foundation’s campaign for real milk website. They tell you what the raw milk laws in each state are, and where to find local farmers selling the stuff. It’s worth it.
Get some glycine. Collagen, found in bones, trachea, bone broth, is the richest source of glycine on the planet. This little amino acid is critically important for metabolic health, and most people are not getting enough.93 It plays many roles in the body as a neurotransmitter and essential component of our skin, bone, and most other tissues. It also has anti-inflammatory effects in the female reproductive tract.94 You need about 10 grams of glycine per day,93 which can be obtained with 20–30 grams of hydrolyzed collagen or several cups of bone broth.
Eat enough calories. If you don’t have weight to lose, then you need to be sure to eat enough calories every day. Chronic undereating when you’re already at a healthy body weight gives off starvation signals that have the body focus on survival rather than reproduction. So, it lowers thyroid activity, growth hormones, testosterone, and the urge to be active.95 In women, chronic undereating can result in amenorrhea, or the loss of periods — this signals infertility.96,97
References
1. Thoma, M. E. et al. Prevalence of infertility in the United States as estimated by the current duration approach and a traditional constructed approach. Fertil. Steril. 99, 1324–1331.e1 (2013).
2. Salas-Huetos, A., Bulló, M. & Salas-Salvadó, J. Dietary patterns, foods and nutrients in male fertility parameters and fecundability: a systematic review of observational studies. Hum. Reprod. Update 23, 371–389 (2017).
3. Anderson, J. E., Farr, S. L., Jamieson, D. J., Warner, L. & Macaluso, M. Infertility services reported by men in the United States: national survey data. Fertil. Steril. 91, 2466–2470 (2009).
4. Carlsen, E., Giwercman, A., Keiding, N. & Skakkebaek, N. E. Evidence for decreasing quality of semen during past 50 years. BMJ 305, 609–613 (1992).
5. Jungwirth, A. et al. European Association of Urology guidelines on Male Infertility: the 2012 update. Eur. Urol. 62, 324–332 (2012).
6. Panth, N., Gavarkovs, A., Tamez, M. & Mattei, J. The Influence of Diet on Fertility and the Implications for Public Health Nutrition in the United States. Front Public Health 6, 211 (2018).
7. Gaskins, A. J. & Chavarro, J. E. Diet and fertility: a review. Am. J. Obstet. Gynecol. 218, 379–389 (2018).
8. Best, D., Avenell, A. & Bhattacharya, S. How effective are weight-loss interventions for improving fertility in women and men who are overweight or obese? A systematic review and meta-analysis of the evidence. Hum. Reprod. Update 23, 681–705 (2017).
9. Wiegner, L., Hange, D., Björkelund, C. & Ahlborg, G., Jr. Prevalence of perceived stress and associations to symptoms of exhaustion, depression and anxiety in a working age population seeking primary care--an observational study. BMC Fam. Pract. 16, 38 (2015).
10. Janevic, T. et al. Effects of work and life stress on semen quality. Fertil. Steril. 102, 530–538 (2014).
11. Nordkap, L. et al. Psychological stress and testicular function: a cross-sectional study of 1,215 Danish men. Fertil. Steril. 105, 174–87.e1–2 (2016).
12. Gollenberg, A. L. et al. Semen quality in fertile men in relation to psychosocial stress. Fertil. Steril. 93, 1104–1111 (2010).
13. Joo, K. J., Kwon, Y. W., Myung, S. C. & Kim, T. H. The effects of smoking and alcohol intake on sperm quality: light and transmission electron microscopy findings. J. Int. Med. Res. 40, 2327–2335 (2012).
14. Sharma, R., Harlev, A., Agarwal, A. & Esteves, S. C. Cigarette Smoking and Semen Quality: A New Meta-analysis Examining the Effect of the 2010 World Health Organization Laboratory Methods for the Examination of Human Semen. Eur. Urol. 70, 635–645 (2016).
15. Van Heertum, K. & Rossi, B. Alcohol and fertility: how much is too much? Fertil Res Pract 3, 10 (2017).
16. Weston A Price Foundation. Francis M. Pottenger, MD - The Weston A. Price Foundation. The Weston A. Price Foundation (2000). Available at: https://www.westonaprice.org/health-topics/nutrition-greats/francis-m-pottenger-md/. (Accessed: 19th September 2018)
17. Spielmann, K. A. A review: Dietary restrictions on hunter-gatherer women and the implications for fertility and infant mortality. Hum. Ecol. 17, 321–345 (1989).
18. Cowlishaw, G. The Determinants Of Fertility Among Australian Aborigines. Mankind 13, 37–55 (1981).
19. Ames, B. N. Low micronutrient intake may accelerate the degenerative diseases of aging through allocation of scarce micronutrients by triage. Proc. Natl. Acad. Sci. U. S. A. 103, 17589–17594 (2006).
20. Price, W. Nutrition and Physical Degeneration: A Comparison of Primitive and Modern Diets and Their Effects (Hardback). (2010).
21. Anez-Bustillos, L. et al. Redefining essential fatty acids in the era of novel intravenous lipid emulsions. Clin. Nutr. 37, 784–789 (2018).
22. Jiang, J. et al. Effect of Marine-Derived n-3 Polyunsaturated Fatty Acids on Major Eicosanoids: A Systematic Review and Meta-Analysis from 18 Randomized Controlled Trials. PLoS One 11, e0147351 (2016).
23. Li, K., Huang, T., Zheng, J., Wu, K. & Li, D. Effect of marine-derived n-3 polyunsaturated fatty acids on C-reactive protein, interleukin 6 and tumor necrosis factor α: a meta-analysis. PLoS One 9, e88103 (2014).
24. Serhan, C. N. Systems approach to inflammation resolution: identification of novel anti-inflammatory and pro-resolving mediators. J. Thromb. Haemost. 7 Suppl 1, 44–48 (2009).
25. Weiss, G., Goldsmith, L. T., Taylor, R. N., Bellet, D. & Taylor, H. S. Inflammation in reproductive disorders. Reprod. Sci. 16, 216–229 (2009).
26. Safarinejad, M. R., Hosseini, S. Y., Dadkhah, F. & Asgari, M. A. Relationship of omega-3 and omega-6 fatty acids with semen characteristics, and anti-oxidant status of seminal plasma: a comparison between fertile and infertile men. Clin. Nutr. 29, 100–105 (2010).
27. Hosseini, B. et al. The Effect of Omega-3 Fatty Acids, EPA, and/or DHA on Male Infertility: A Systematic Review and Meta-analysis. J. Diet. Suppl. 1–12 (2018).
28. Greenberg, J. A., Bell, S. J. & Van Ausdal, W. Omega-3 Fatty Acid supplementation during pregnancy. Rev. Obstet. Gynecol. 1, 162–169 (2008).
29. Swanson, D., Block, R. & Mousa, S. A. Omega-3 fatty acids EPA and DHA: health benefits throughout life. Adv. Nutr. 3, 1–7 (2012).
30. Derbyshire, E. Brain Health across the Lifespan: A Systematic Review on the Role of Omega-3 Fatty Acid Supplements. Nutrients 10, (2018).
31. Borel, P. & Desmarchelier, C. Genetic Variations Associated with Vitamin A Status and Vitamin A Bioavailability. Nutrients 9, (2017).
32. Amann, P. M., Eichmüller, S. B., Schmidt, J. & Bazhin, A. V. Regulation of gene expression by retinoids. Curr. Med. Chem. 18, 1405–1412 (2011).
33. Theodosiou, M., Laudet, V. & Schubert, M. From carrot to clinic: an overview of the retinoic acid signaling pathway. Cell. Mol. Life Sci. 67, 1423–1445 (2010).
34. Jauregui, E. J., Mitchell, D., Topping, T., Hogarth, C. A. & Griswold, M. D. Retinoic acid receptor signaling is necessary in steroidogenic cells for normal spermatogenesis and epididymal function. Development 145, (2018).
35. Clagett-Dame, M. & Knutson, D. Vitamin A in reproduction and development. Nutrients 3, 385–428 (2011).
36. Field, C. J., Johnson, I. R. & Schley, P. D. Nutrients and their role in host resistance to infection. J. Leukoc. Biol. 71, 16–32 (2002).
37. Zimmermann, M. B. Interactions of vitamin A and iodine deficiencies: effects on the pituitary-thyroid axis. Int. J. Vitam. Nutr. Res. 77, 236–240 (2007).
38. Verma, I., Sood, R., Juneja, S. & Kaur, S. Prevalence of hypothyroidism in infertile women and evaluation of response of treatment for hypothyroidism on infertility. Int J Appl Basic Med Res 2, 17–19 (2012).
39. Nikoobakht, M. R. et al. The role of hypothyroidism in male infertility and erectile dysfunction. Urol. J. 9, 405–409 (2012).
40. Aghajafari, F. et al. Association between maternal serum 25-hydroxyvitamin D level and pregnancy and neonatal outcomes: systematic review and meta-analysis of observational studies. BMJ 346, f1169 (2013).
41. Grzechocinska, B., Dabrowski, F. A., Cyganek, A. & Wielgos, M. The role of vitamin D in impaired fertility treatment. Neuro Endocrinol. Lett. 34, 756–762 (2013).
42. Lerchbaum, E. & Obermayer-Pietsch, B. Vitamin D and fertility: a systematic review. Eur. J. Endocrinol. 166, 765–778 (2012).
43. Muscogiuri, G. et al. Shedding new light on female fertility: The role of vitamin D. Rev. Endocr. Metab. Disord. 18, 273–283 (2017).
44. Lerchbaum, E. & Rabe, T. Vitamin D and female fertility. Curr. Opin. Obstet. Gynecol. 26, 145–150 (2014).
45. Viswanathan, M. et al. Folic Acid Supplementation for the Prevention of Neural Tube Defects: An Updated Evidence Report and Systematic Review for the US Preventive Services Task Force. JAMA 317, 190–203 (2017).
46. Caudill, M. A. Pre- and postnatal health: evidence of increased choline needs. J. Am. Diet. Assoc. 110, 1198–1206 (2010).
47. Zeisel, S. H. Importance of methyl donors during reproduction. Am. J. Clin. Nutr. 89, 673S–7S (2009).
48. Fischer, L. M. et al. Sex and menopausal status influence human dietary requirements for the nutrient choline. Am. J. Clin. Nutr. 85, 1275–1285 (2007).
49. Zeisel, S. H. Choline: critical role during fetal development and dietary requirements in adults. Annu. Rev. Nutr. 26, 229–250 (2006).
50. Burke, R. M., Leon, J. S. & Suchdev, P. S. Identification, prevention and treatment of iron deficiency during the first 1000 days. Nutrients 6, 4093–4114 (2014).
51. Picciano, M. F. Pregnancy and lactation: physiological adjustments, nutritional requirements and the role of dietary supplements. J. Nutr. 133, 1997S–2002S (2003).
52. Gambling, L., Lang, C. & McArdle, H. J. Fetal regulation of iron transport during pregnancy. Am. J. Clin. Nutr. 94, 1903S–1907S (2011).
53. Bothwell, T. H. Iron requirements in pregnancy and strategies to meet them. Am. J. Clin. Nutr. 72, 257S–264S (2000).
54. Beaton, G. H. Iron needs during pregnancy: do we need to rethink our targets? Am. J. Clin. Nutr. 72, 265S–271S (2000).
55. Fallah, A., Mohammad-Hasani, A. & Colagar, A. H. Zinc is an Essential Element for Male Fertility: A Review of Zn Roles in Men’s Health, Germination, Sperm Quality, and Fertilization. J Reprod Infertil 19, 69–81 (2018).
56. Colagar, A. H., Marzony, E. T. & Chaichi, M. J. Zinc levels in seminal plasma are associated with sperm quality in fertile and infertile men. Nutr. Res. 29, 82–88 (2009).
57. Morton, A. Hypomagnesaemia and pregnancy. Obstet Med 11, 67–72 (2018).
58. Zarean, E. & Tarjan, A. Effect of Magnesium Supplement on Pregnancy Outcomes: A Randomized Control Trial. Adv. Biomed. Res. 6, 109 (2017).
59. Maggio, M. et al. The Interplay between Magnesium and Testosterone in Modulating Physical Function in Men. Int. J. Endocrinol. 2014, 525249 (2014).
60. Wilcox, A. J., Weinberg, C. R. & Baird, D. D. Timing of sexual intercourse in relation to ovulation. Effects on the probability of conception, survival of the pregnancy, and sex of the baby. N. Engl. J. Med. 333, 1517–1521 (1995).
61. Hampton, K. D., Mazza, D. & Newton, J. M. Fertility-awareness knowledge, attitudes, and practices of women seeking fertility assistance. J. Adv. Nurs. 69, 1076–1084 (2013).
62. Hampton, K. & Mazza, D. Fertility-awareness knowledge, attitudes and practices of women attending general practice. Aust. Fam. Physician 44, 840–845 (2015).
63. Freis, A. et al. Plausibility of Menstrual Cycle Apps Claiming to Support Conception. Front Public Health 6, 98 (2018).
64. Zhu, B. P., Rolfs, R. T., Nangle, B. E. & Horan, J. M. Effect of the interval between pregnancies on perinatal outcomes. N. Engl. J. Med. 340, 589–594 (1999).
65. Kangatharan, C., Labram, S. & Bhattacharya, S. Interpregnancy interval following miscarriage and adverse pregnancy outcomes: systematic review and meta-analysis. Hum. Reprod. Update 23, 221–231 (2017).
66. Palmery, M., Saraceno, A., Vaiarelli, A. & Carlomagno, G. Oral contraceptives and changes in nutritional requirements. Eur. Rev. Med. Pharmacol. Sci. 17, 1804–1813 (2013).
67. Mima, M., Greenwald, D. & Ohlander, S. Environmental Toxins and Male Fertility. Curr. Urol. Rep. 19, 50 (2018).
68. Sengupta, P. & Banerjee, R. Environmental toxins: alarming impacts of pesticides on male fertility. Hum. Exp. Toxicol. 33, 1017–1039 (2014).
69. Mehrpour, O., Karrari, P., Zamani, N., Tsatsakis, A. M. & Abdollahi, M. Occupational exposure to pesticides and consequences on male semen and fertility: a review. Toxicol. Lett. 230, 146–156 (2014).
70. Noorimotlagh, Z., Haghighi, N. J., Ahmadimoghadam, M. & Rahim, F. An updated systematic review on the possible effect of nonylphenol on male fertility. Environ. Sci. Pollut. Res. Int. 24, 3298–3314 (2017).
71. Estill, M. S. & Krawetz, S. A. The Epigenetic Consequences of Paternal Exposure to Environmental Contaminants and Reproductive Toxicants. Curr Environ Health Rep 3, 202–213 (2016).
72. Vandenberg, L. N. et al. Hormones and endocrine-disrupting chemicals: low-dose effects and nonmonotonic dose responses. Endocr. Rev. 33, 378–455 (2012).
73. Yi, H. et al. A pilot study on association between phthalate exposure and missed miscarriage. Eur. Rev. Med. Pharmacol. Sci. 20, 1894–1902 (2016).
74. Joensen, U. N. et al. Phthalate excretion pattern and testicular function: a study of 881 healthy Danish men. Environ. Health Perspect. 120, 1397–1403 (2012).
75. Kappeler, C. J. & Hoyer, P. B. 4-vinylcyclohexene diepoxide: a model chemical for ovotoxicity. Syst. Biol. Reprod. Med. 58, 57–62 (2012).
76. Bolden, A. L., Rochester, J. R., Schultz, K. & Kwiatkowski, C. F. Polycyclic aromatic hydrocarbons and female reproductive health: A scoping review. Reprod. Toxicol. 73, 61–74 (2017).
77. Madeen, E. P. & Williams, D. E. Environmental PAH exposure and male idiopathic infertility: a review on early life exposures and adult diagnosis. Rev. Environ. Health 32, 73–81 (2017).
78. Bondy, S. C. & Campbell, A. Water Quality and Brain Function. Int. J. Environ. Res. Public Health 15, (2017).
79. Adams, J. A., Galloway, T. S., Mondal, D., Esteves, S. C. & Mathews, F. Effect of mobile telephones on sperm quality: a systematic review and meta-analysis. Environ. Int. 70, 106–112 (2014).
80. Liu, K. et al. Association between mobile phone use and semen quality: a systemic review and meta-analysis. Andrology 2, 491–501 (2014).
81. Cook, H. J., Steneck, N. H., Vander, A. J. & Kane, G. L. Early research on the biological effects of microwave radiation: 1940-1960. Ann. Sci. 37, 323–351 (1980).
82. Durairajanayagam, D., Agarwal, A. & Ong, C. Causes, effects and molecular mechanisms of testicular heat stress. Reprod. Biomed. Online 30, 14–27 (2015).
83. Garolla, A. et al. Seminal and molecular evidence that sauna exposure affects human spermatogenesis. Hum. Reprod. 28, 877–885 (2013).
84. Rao, M. et al. Effect of transient scrotal hyperthermia on sperm parameters, seminal plasma biochemical markers, and oxidative stress in men. Asian J. Androl. 17, 668–675 (2015).
85. Kloss, J. D., Perlis, M. L., Zamzow, J. A., Culnan, E. J. & Gracia, C. R. Sleep, sleep disturbance, and fertility in women. Sleep Med. Rev. 22, 78–87 (2015).
86. Piché, M.-L., Babineau, V., Robitaille, J., Lachance, É. & Ruchat, S.-M. Lifestyle-Related Factors Associated with Reproductive Health in Couples Seeking Fertility Treatments: Results of A Pilot Study. Int J Fertil Steril 12, 19–26 (2018).
87. Danilenko, K. V., Sergeeva, O. Y. & Verevkin, E. G. Menstrual cycles are influenced by sunshine. Gynecol. Endocrinol. 27, 711–716 (2011).
88. Danilenko, K. V. & Samoilova, E. A. Stimulatory effect of morning bright light on reproductive hormones and ovulation: results of a controlled crossover trial. PLoS Clin. Trials 2, e7 (2007).
89. Stang, J. & Huffman, L. G. Position of the Academy of Nutrition and Dietetics: Obesity, Reproduction, and Pregnancy Outcomes. J. Acad. Nutr. Diet. 116, 677–691 (2016).
90. Harrison, C. L., Brown, W. J., Hayman, M., Moran, L. J. & Redman, L. M. The Role of Physical Activity in Preconception, Pregnancy and Postpartum Health. Semin. Reprod. Med. 34, e28–37 (2016).
91. Orio, F. et al. Effects of physical exercise on the female reproductive system. Minerva Endocrinol. 38, 305–319 (2013).
92. Malekinejad, H. & Rezabakhsh, A. Hormones in Dairy Foods and Their Impact on Public Health - A Narrative Review Article. Iran. J. Public Health 44, 742–758 (2015).
93. Meléndez-Hevia, E., De Paz-Lugo, P., Cornish-Bowden, A. & Cárdenas, M. L. A weak link in metabolism: the metabolic capacity for glycine biosynthesis does not satisfy the need for collagen synthesis. J. Biosci. 34, 853–872 (2009).
94. Laschke, M. W., Schwender, C., Scheuer, C., Vollmar, B. & Menger, M. D. Dietary glycine does not affect physiological angiogenesis and reproductive function, but inhibits apoptosis in endometrial and ovarian tissue by down-regulation of nuclear factor-kappaB. Fertil. Steril. 90, 1460–1469 (2008).
95. Redman, L. M. & Ravussin, E. Caloric restriction in humans: impact on physiological, psychological, and behavioral outcomes. Antioxid. Redox Signal. 14, 275–287 (2011).
96. Klein, D. A. & Poth, M. A. Amenorrhea: an approach to diagnosis and management. Am. Fam. Physician 87, 781–788 (2013).
97. Thein-Nissenbaum, J. & Hammer, E. Treatment strategies for the female athlete triad in the adolescent athlete: current perspectives. Open Access J Sports Med 8, 85–95 (2017).